Genetic Variants May Disrupt Myelin Production
Among Alzheimer ‘s victims, 40% to 65% have a genetic variant called APOE4. Scientists have long known that this variant significantly increases the risk of neurodegenerative diseases, especially when one inherits a copy of APOE4 from both parents, but they are still learning to explain the molecular mechanisms of APOE4 action.
A study published in the November 16 issue of Nature suggests that APOE4 may lead to Alzheimer’s disease in a way that leads to cholesterol accumulation in oligodendrocytes and reduces the ability of cells to perform their main function: fat myelin sheaths that protect neurons and help them transmit signals. It was further found that in mice carrying APOE4, removing blocked cholesterol, the main component of myelin, and allowing this substance to cross the cell membrane partially restored myelin production and improved cognitive performance, suggesting that this is a therapeutic target against Alzheimer’s disease.
“They showed that one thing apolipoprotein E does is that it seems to affect lipid metabolism in oligodendrocytes, which has not been described as much before,” says David Holtzman, a neurologist at Washington University in St. Louis, who was not involved in the study. Holtzman says others have shown that APOE4 can affect lipids and cholesterol in many different cell types, particularly microglia and astrocytes, “but as far as I know, no one has really focused specifically on oligodendrocytes.”
“Many biological pathways are disturbed by APOE4,” says Li-Huei Tsai, a neuroscientist at the Picol Institute for Learning and Memory at MIT and co-author of the study. Because the APOE gene encodes a protein responsible for transporting lipids between cells, Tsai says the researchers decided to focus on how this variant disrupts the metabolism of cholesterol and other lipids.
By transcriptome analysis, the researchers compared postmortem brain tissue from Alzheimer’s patients with non-Alzheimer’s patients and measured various gene expression levels in those with 0, 1, or 2 APOE4 variants, and showed that “APOE4 has a huge impact on gene expression,” Tsai said, especially on many genes that affect lipids. She says a similar analysis of oligodendrocytes found that genes associated with making cholesterol were significantly upregulated in cells, while genes associated with making myelin were downregulated.
“What we see from gene expression data is counterintuitive,” says Manolis Kellis, a computational biologist at the Massachusetts Institute of Technology Computer Science and Artificial Intelligence Laboratory and co-author of the study, adding that signals appear to be mismatched because the regulatory directions of the genome are different.
To delve into this mystery, the researchers performed lipid analysis of brain tissue from people carrying at least one APOE4 or APOE3 gene. APOE4 or APOE3 are the most common APOE gene variants and are not associated with an increased risk of Alzheimer’s disease. The results showed higher levels of cholesteryl esters in APOE4 brains, which Tsai says are insoluble cholesterol known to accumulate intracellularly. When the researchers stained human and mouse brain tissue homozygous for APOE4, they found that cholesterol droplets accumulated within oligodendrocytes in both. Also, cholesterol was more prevalent extracellularly in samples containing APOE3.
The researchers began to suspect that APOE4 variants hindered cholesterol trafficking through oligodendrocyte membranes. Imagine that oligodendrocytes work like myelin printers, and the emerging hypothesis is that these cells have large amounts of ink (cholesterol), but the ink is stuck in the ink box.
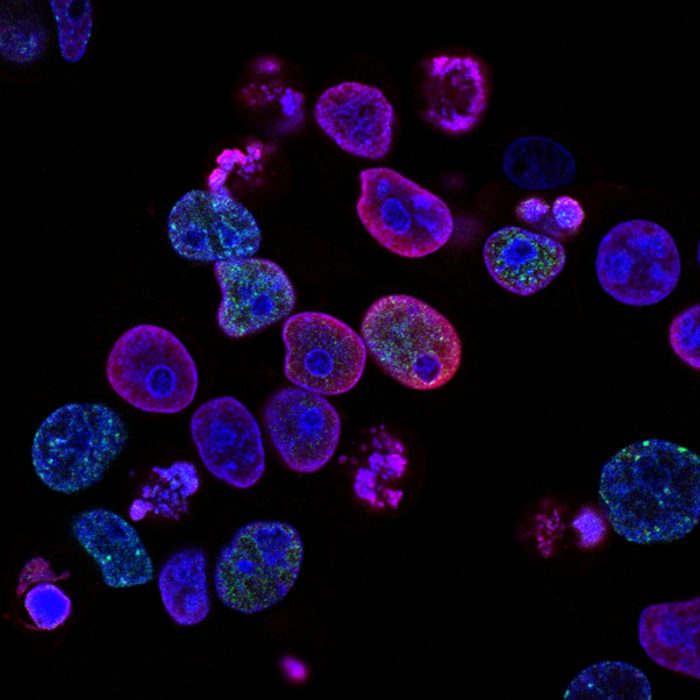
To test the relationship between APOE4 and reduced myelin production, the investigators performed a wide variety of experiments. First, they induced pluripotent stem cells to form oligodendrocytes (precursors of oligodendrocytes), which were then co-cultured with laboratory-induced neurons. Typically, these co-cultured oligodendrocytes begin to form myelin within a few weeks, Tsai says. The researchers noticed this effect in APOE3 co-cultures, “but in APOE4 co-cultures, we saw a great reduction … characteristic of myelin basic protein,” which suggests less myelin production. Transmission electron microscopy of brain tissue also showed that mice carrying APOE4 had fewer neurons with myelinated axons, and that myelinated neuronal sheaths were thinner than those carrying APOE3.
The team then tried to reduce cholesterol accumulation and restore myelin production using cyclodextrin, a drug known to reduce intracellular cholesterol accumulation, in vitro and in APOE4 mice. Treatment of APOE4 oligodendrocyte-neuron co-cultures with cyclodextrin increased myelin to levels close to APOE3 co-cultures after two weeks. The researchers injected the drug subcutaneously twice a week for 8 weeks and then compared their brain tissue with mice that did not receive APOE4 treatment. Cholesterol accumulation within oligodendrocytes was reduced in treated mice, and the researchers observed increased levels of extracellular myelin basic protein, suggesting that treatment improved cholesterol flow and myelination. Finally, the researchers administered several cognitive tests to mice, “What we see is, indeed, that it improves cognitive performance.”
Holtzman said he wanted to see others confirm the results, and he did not believe the findings were clinically relevant to humans. “There are many mechanisms for how APOE4 alters the risk of Alzheimer ‘s disease,” he said. “I am not sure if this is one of the important mechanisms. This is really hard to judge.” Changes in cholesterol and myelin have the potential to lead to decline or degeneration associated with Alzheimer’s disease, he said. “But we know APOE has done a lot of other things that have a huge impact on the pathology of Alzheimer’s disease, and these effects are not related to these findings.”
Although APOE4 is associated with an increased risk of Alzheimer’s disease and a steep decline in cognitive performance following the onset of symptoms, “these effects of APOE4 on Alzheimer’s disease can only be seen in the presence of Alzheimer’s pathology”, particularly the typical accumulation of amyloid plaques in the brain or intraneuronal tau tangles. He added that APOE4 is not known to affect myelin levels in adults without Alzheimer’s disease, and to his knowledge no one has investigated this possibility. Thus, in APOE4 mice without Alzheimer’s disease, it was found that myelin reduction and cyclodextrin-mediated myelin and cognitive recovery may or may not be clinically relevant to humans, he said.
Tsai explained via email that past functional magnetic resonance imaging studies have linked genetic variants to white matter reduction, which is mainly composed of myelinated nerve axons. She added that her work with her colleagues highlighted the need to investigate Alzheimer’s disease risk mechanisms that may begin before disease and cognitive decline begin. “Our findings suggest earlier opportunities for therapeutic intervention,” she said. “I think this is what makes this study interesting.”
Tsai says her laboratory will not be involved in any potential clinical trials to explore whether cyclodextrin helps reduce symptoms in people with Alzheimer’s disease. Instead, she and her colleagues will continue to investigate the mechanisms behind the effects of genetic variants leading to oligodendrocyte obstruction. “The more we understand how (cholesterol) reaches there, the more potential drug discovery targets will emerge.”